Sterilizing and Reusing N95 Respirators
- By : PureAire Monitoring Systems
- Posted on : April 16, 2020
- News Room
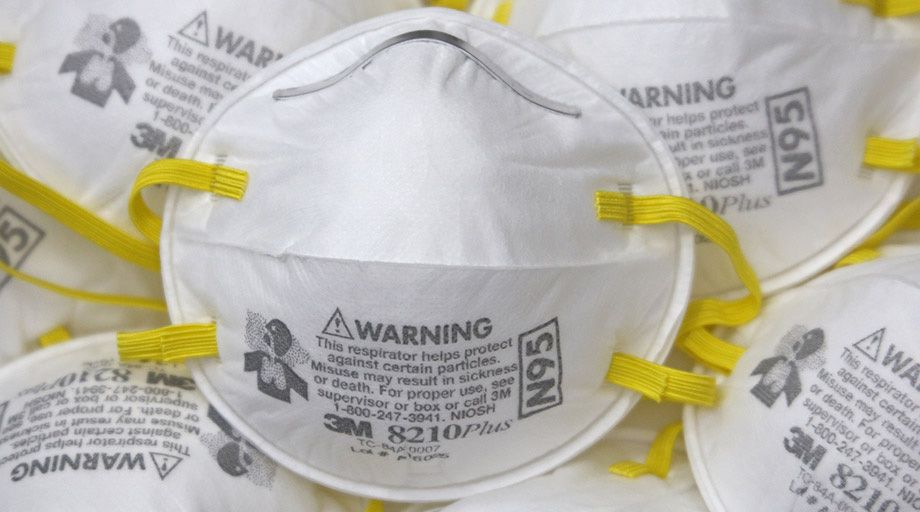
Personal protection equipment (“PPE”)includes the gloves, gowns, N95 respiratory masks, and other items required by doctors, nurses, and other healthcare personnel responsible for treating patients, including those suffering from infectious diseases. As has become evident in the current COVID-19 emergency affecting the globe, during a crisis, these critical items may not always be available in the quantities needed to meet the challenge of treating large numbers of sick people.
Among the most sought after PPE items today are N95 respirators. According to the U.S. Food and Drug Administration (“FDA”), N95 respirators are essential gear to protect the wearer from airborne particles and to keep liquid materials from contaminating the wearer’s face. Now, more than ever, there is a need for readily available, sterile N95 respirators.
Challenge/Solution
Thus far, during the COVID-19 pandemic, we have witnessed a desperate struggle by public and private sector entities to keep up with the huge increase in N95 respirator usage which, in turn, has at times left healthcare workers and other front-line personnel without the equipment necessary to safely do their jobs. Traditionally, N95 respirators have been discarded after a single use and, while on-shore production has recently ramped up, demand for the masks far outstrips supply during the present period in which the number of COVID-19 cases surges daily.
Fortunately, as medical providers and first responders scramble to procure the safety products required to attend to the patients in their care, businesses are innovating to meet the significant challenge posed by the current respirator supply/demand mismatch.
For instance, in late March of 2020, Battelle, a Columbus, OH-based nonprofit research and development firm, received FDA approval for its Critical Care Decontamination System (“CCDS”) process for decontaminating, on a very large scale, the N95 face masks used by healthcare providers. The CCDS process involves pumping concentrated hydrogen peroxide vapor (H2O2) into so-called decontamination chambers (20-foot shipping containers fitted with racks on which the N95 masks are hung) for a 2 ½ hour decontamination cycle. So long as the masks have not been heavily soiled, the CCDS process will allow each N95 respirator to be sterilized and reused up to 20 times. The system is highly scalable, and Battelle, which intends to deploy CCDS as needed throughout the U.S., believes that its larger versions should be capable of sterilizing up to 80,000 N95 masks per day.
Additionally, in early April, the FDA granted STERIS, another Ohio-based company, an Emergency Use Authorization (“EUA”) to begin, on a temporary basis, small-scale N95 sterilization, pursuant to which certain of the company’s V-PRO Low-Temperature Sterilization System machines are approved to sterilize up to 10 masks apiece per 28 minute vaporized hydrogen peroxide sterilization cycle. STERIS reportedly has 100 such V-PRO machines across the State of Ohio which have the capacity to sterilize N95 respirators as provided for in the EUA, and each re-sterilized mask is reusable up to 10 times by repeating the V-PRO process.
Hydrogen Peroxide Vapor
Hydrogen peroxide vapor (“H2O2”)is a widely used gaseous sterilant that has been shown to be effective in killing viruses, fungi, bacteria, and other pathogens, and H2O2 decontamination is a standard process used in pharmaceutical, research, and medical facilities.H2O2 vapor works by breaking apart the outer membranes of the pathogen to which it is applied, thereby destroying the dangerous microorganism.
Hydrogen peroxide is a colorless gas with a sharp odor. Exposure to H2O2 can irritate the eyes, nose, throat and skin, as well as cause headaches, dizziness, nausea, and vomiting. Long-term exposure can negatively affect the lungs, producing coughing and shortness of breath, and elevated levels of hydrogen peroxide may result in a build-up of fluid in the lungs (a dangerous condition known as pulmonary edema). The current OSHA permissible exposure limit (PEL) standard is 1 part of hydrogen peroxide parts per million(ppm).
Gas Detection is Crucial for Personnel Safety
Facilities using concentrated hydrogen peroxide vapor to decontaminate PPE or other medical equipment need to ensure that employees are not exposed to H2O2 at levels greater than OSHA’s PEL of 1ppm. Since it is always present, the odor from H2O2 vapor does not provide warning that hazardous H2O2 concentrations may exist. Therefore, in the absence of appropriate monitoring, it is impossible to determine whether hydrogen peroxide concentrations are approaching dangerous levels.
Best practices call for the installation of hydrogen peroxide monitors anywhere H2O2 is stored or used.
PureAire Monitors
 PureAire Monitoring Systems’ Universal Gas Detectors use “smart” sensor cell technology to continuously track levels of ammonia, bromine, hydrogen, hydrogen chloride, and other toxic gases, including hydrogen peroxide. The sensor cell is programmed to monitor for a specific gas and measurement range, as required by the user.
PureAire Monitoring Systems’ Universal Gas Detectors use “smart” sensor cell technology to continuously track levels of ammonia, bromine, hydrogen, hydrogen chloride, and other toxic gases, including hydrogen peroxide. The sensor cell is programmed to monitor for a specific gas and measurement range, as required by the user.
PureAire’s Universal Gas Detectors allow operators of medical decontamination facilities and systems to detect elevated hydrogen peroxide levels before employee health is put at risk. In the event that H2O2 is elevated to an unsafe level, the Universal Gas Detector will set off an alarm that includes horns and flashing lights, alerting staff to vacate the affected area.
The Universal Gas Detector’s easy to read screen makes it simple for employees to monitor hydrogen peroxide levels at a glance, providing them with the assurance that their health is not jeopardized while they perform their important work.